Choudhary Medical Clinic, 1st Floor, Parekh House, Gandhibagh, Nagpur - 2
1. Exercise testing in assessment and management of Patients in Clinical Practice - Present situation
By Prof Dr Sumer S Choudhary , Sanjiw Choudhary
Key words : Exercise; heart; Interpretation; methodology; 6min walk test; testing
[Downloaded free from http://www.lungindia.com on Friday, October 10, 2014, IP: 117.211.27.59]
2. Sleep effects on breathing and respiratory diseases
By Prof Dr Sumer S Choudhary , Sanjiw R. Choudhary
Key Words: Asthma, COPD, neuromuscular, sleep
ABSTRACT
To understand normal sleep pattern and physiological changes during sleep, sleep and breathing interaction,
nomenclature and scales used in sleep study, discuss the effect of rapid eye movements and non-rapid eye movements
while sleep and to review the effects of obstructive and restrictive lung disease on gas exchange during sleep and
sleep architecture.
[Downloaded free from http://www.lungindia.com on Friday, October 10, 2014, IP: 117.211.27.59]
3. Polysomnography: A Useful Tool in Diagnosis And Management Of Sleep Diseases
By Prof Dr. Sumer S Choudhary
ABSTRACT
Sleep diseases, of which obstructive sleep apnea is one, are one of the leading health problems in both developed and developing countries. However, education and awareness regarding diagnosis and management is still lacking among both public and treating physician. The initial work done on sleep study was done in the era of Rechtschaffen and Kates. Presently Computerized Polysomnography (PSG) incorporated with different channels is an important tool in management of patients of sleep disorders. Any sleep study which is to be performed requires a well equipped and validated sleep laboratory for proper results and interpretation of data. Nomenclatures are defined, scales have been formulated and grading of disease on the basis of PSG study has been done. Different types of sleep study like study in sleep centre, Multiple sleep latency test, maintenance of wakefulness test, and portable home monitoring tests are done routinely of which portable home based test is not encouraged. It not only helps in detecting obstructive sleep apnea but is also helpful in the management of central sleep apnea patients. Key Words : Polymnography, sleep staging, apnea
http://www.pjms.in/index.php/panacea/search/search - Prof Dr Sumer Sanjiv Choudhary
4. Efficacy and treatment outcome of DOTS in RNTCP
Prof Dr Sumer Sanjiv Choudhary, B Tayade, Pinky Keshwani
ABSTRACT
Retrospective observation analysis was carried out to evaluate the outcome of DOTS under RNTCP at NKP Salve Institute of Medical Sciences and Lata Mangeshkar Hospital Digdoh Hills Hingna Nagpur tertiary care center . Total 141 patients were studied under all the categories registered from October 2006 to February 2008 with a follow up of one year . Standard norms were applied for treating and registering under different categories and for outcome of treatment. Category 1 consisted of 96 patients category 2 constituted 12 patients and category 3 had 33 patients. All patients were closely followed up during treatment phase and were asked for a regular follow up after completion of treatment. Of the 141 patients 94.33% patients were declared cured/ treatment completed, 3.54% defaulted, the failure rate was 1.418% and overall death rate was 2.128%. The cure / treatment completion in present study is 97.67% and 75% for new smear positive and pretreatment patients. Success rate in terms of cure/ treatment completion is much higher in category 1 patients and slightly higher in category 2 patients as compared to the national average of 86.50% and 70.5% in new smear positive and retreatment cases respectively . This was comparable to the other studies published earlier .
Keywords: DOTS, RNTCP , Outcome, Enhanced.
http://www.pjms.in/index.php/panacea/search/search - Prof Dr Sumer Sanjiv Choudhary
5. Non-invasive mechanical ventilation in clinical practicecons pros and cons
Prof Dr Sumer Sanjiv Choudhary
ABSTRACT
Noninvasive positive-pressure ventilation is a type of mechanical ventilation that does not require an artificial airway . Studies published in the 1990s that evaluated the efficacy of this technique for the treatment of diseases like chronic obstructive pulmonary disease, congestive heart failure and acute respiratory failure have generalized its use in recent years. Important issues include the selection of the type of ventilation interface and the type of
ventilator .
Currently available interfaces include nasal, oro-nasal and facial masks, mouthpieces and helmets. Comparisons of the available interfaces have not found any one of them to be superior . Both critical care ventilators and portable ventilators can be used for noninvasive positive-pressure ventilation; however , the choice of ventilator type depends on the patient's condition and therapeutic requirements. The best results (decreased need for intubations and decreased mortality) have been reported among patients with exacerbations of chronic obstructive pulmonary disease and cardiogenic pulmonary edema.
Key Words: Non Invasive, Mechanical Ventilation, Respiratory, Interfaces.
http://www.pjms.in/index.php/panacea/search/search - Prof Dr Sumer Sanjiv Choudhary
6. Pulmonary function tests in clinical practice: importance, requirements and limitations
Prof Dr Sumer Sanjiv Choudhary
ABSTRACT
Pulmonary function tests have progressed from initially used water seal types to modern era electronic computerized versions. The newer software are comparatively easier to operate and less time consuming. They are patient friendly and easier to understand. However there are limitations to pulmonary function tests, as the pattern of abnormality indicates type of problem however they do not provide anatomic diagnosis. Battery of tests is available which help in evaluation of different aspects of pulmonary function. It is possible to monitor the progression of disease and effect of management. However no single test can evaluate all aspects of pulmonary function. Pulmonary function test can be carried out at bedside in critically ill patients with the help of portable spirometers in addition to the routine clinical tests. Commonly performed pulmonary function tests are dynamic studies –pre and post bronchodilator tests, evaluation of lung volumes with body plethysmography , nitrogen washout or helium dilution methods, diffusion capacity of the lung carbon monoxide by single breath analysis, arterial blood gases and pulse oximetry . Other commonly performed tests are maximal expiratory and inspiratory pressure, exercise induced(T readmill)or allergen induced bronchoprovocative tests, shunt studies and Dead space measurements. If the pulmonary function tests are done with quality assurance, validation of the equipment, proper technique, reference values and applying right ethnic correction factors, the data generated are most of the times accurate and reproducible.
http://www.pjms.in/index.php/panacea/search/search - Prof Dr Sumer Sanjiv Choudhary
7. Obstructive sleep apnea therapy: Treatment and reliever in co-morbid diseases
Prof Dr Sumer Sanjiv Choudhary
ABSTRACT
Obstructive sleep apnea (OSA)-induced biological changes include intermittent hypoxia, intermittent hypercapnia, intrathoracic pressure changes, and sympathetic activation and sleep fragmentation. OSA can cause metabolic dysregulation, endothelial dysfunction, systemic inflammation, oxidative stress and hypercoagulation, and neurohumoral changes. Important comorbidities associated with OSA are cardiovascular system i.e. hypertension, cardiac arrhythmias, coronary artery disease, cardiac failure and stroke, respiratory system i.e. pulmonary hypertension, asthma ,COPD, central nervous system i.e. erectile dysfunction, seizure disorders, strokes, psychiatric illness and other systemic diseases like obesity, sudden infant death syndrome, chronic renal failure, diabetes mellitus, GERD. The diagnosis of OSA is based on polysomographic studies. PAP treatment has been found to have beneficial effects in many of these consequences. There is also a need to identify other modalities of treatment. Certainly, the treatment of OSA can greatly improve or even revert some of the co morbid conditions.
Keywords: Sleep apnea, Co-morbid, Asthma, Cardiovascular, Obesity, Diabetes, Epilepsy, GERD, Erectile.
http://www.pjms.in/index.php/panacea/search/search - Prof Dr Sumer Sanjiv Choudhary
8. Prof Dr Sumer Sanjiv Choudhary. Recent Advances In Diagnosis Tuberculosis.Update AFB NEWS The Tuberculosis Bulletin.January To June 2013 Vol 1-Issue 1.Page 25 to 28. Indexed 1SSN 2321-7901 Click Here
9. Prof Dr Sumer Sanjiv Choudhary.Tuberculosis and HIV:Step towards resolving the drug interaction between antiretrovirals and antituberculars. Review Article. AFB News The Tuberculosis Bulletin.July To December 2013 Vol 1-Issue 2.Page 10 to 19. (Indexed 1SSN 2321-7901) - Click Here
10. Prof Dr Sumer Sanjiv Choudhary A Study of Treatment Outcome,Performance and Response of Patients On DOTS under RNTCP Original Article AFB NEWS The Tuberculosis Jan - June 2014, Vol 2 - Issue I Click Here
11. Interstial Lung Diseases [ILD]: Simplified, Advances, What's New
Prof Dr Sumer Sanjiv Choudhary
ABSTRACT
Interstitial lung disease (ILD) is a diverse collection of disorders characterized by impaired gas exchange,restricted physiology on lung function testing, and diffuse parenchymal lung infiltrates on radiography. Although the interstitial lung diseases are many in routine clinical practice, the most commonly encountered in practice are sarcoidosis, idiopathic pulmonary fibrosis (IPF), and connective tissue disease-associated interstitial lung diseases.In immune-compromised patients, infection is the most common cause of diffuse lung infiltrates and must be ruled out before any attempt to treat with immune altering agents like corticosteroids. There are many new agents available for managing ILD, lung transplantation and pulmonary rehabilitation is also available treatment option however we require an orchestrated effort towards simplif ying, for a better understanding and treatment of this complex life threatening group of diseases. This review will focus on the more clinically significant recent advances and recommendations in the field of interstitial lung disease. Recent advances in diagnostic techniques and treatment interventions represent a signi?cant step forward in our understanding and management of ILD.
Keywords: Interstitial lung diseases,Idiopathic pulmonary fibrosis,Lung transplantation,Gap index.
http://www.pjms.in/index.php/panacea/search/search - Prof Dr Sumer Sanjiv Choudhary
12. Outcome And Comparison of Adult and Childhood Tuberculosis in RNTCP: A Retrospective Study
Prof Dr Sumer Sanjiv Choudhary, BO Tayade, Shafee Khan, R Giri, Parthiv Shah, Virag Doshi
ABSTRACT
Retrospective observation analysis from Tuberculosis Unit (T.U.) Nagpur register to evaluate the outcome of DOTS under RNTCP at NKP Salve Institute of Medical Sciences And Lata Mangeshkar Hospital Digdoh Hills Hingna Nagpur a tertiary care centre..Total 545 patients were studied under all the categories registered from January 2009 to December 2013.Standard norms were applied for treating and registering under different categories and for outcome of treatment. The total mean age of patients was 35.11 years (S.D 15.99), the mean of Adult patients were 37.87 years (S.D 14.06) and Paediatric patients were 8.373 years (S.D 4.891). 494 (90.64%) patients were Adults and 51(9.36%) Paediatrics In Adult patients, 449(90.89%) had favorable outcome, 45(9.11%) patients had unfavorable outcome. All 51 (100%) patients in paediatric group had favorable outcomes. Maximum patients were registered under Category 1, i.e 448 patients of which 398 patients were Adults and 50 patients were in Paediatric age group.. Of the 545 patients 337(61.83%) were male and 208((38.17%) were female In both the age groups there were higher number of males compared to females. Of the 545 patients 500(91.74%) patients were declared favorable outcome. 198(95.19%) Females had favorable and 10 (4.81%) had unfavorable outcome.174 were in Adult and 24 in Paediatric age group in favorable outcome of females. 302 (89.61%) Males had favorable of which 275 were Adults and 27 were paediatric and 35 (10.39%) male had unfavorable outcomes all in Adult age group. 391(71.74%) were of pulmonary tuberculosis and 154(28.26%) were of Extra pulmonary Tuberculosis, the ratio between the two was 2.5:1.The ratio of smear positive to smear negative was 1.35:1. 45(8.26%) patients had unfavorable outcomes of which12 (2.2%) defaulted, the failure rate was 0.75%, 4 patients, overall death rate was 18(3.3%), 11(2.05%) patients were transferred out and all Adults. Success rate in terms of cure/treatment completion is 94.19% and 78% is much higher in category 1 patients and slightly higher in category 2 patients as compared to the national average of 86.50% and 70.5% in new respectively. This was comparable to the other studies published earlier. The registration of childhood TB was better than national average. There were differences in presentation and treatment outcomes among children and adult patients. Category 1 and sputum was significant predictor in childhood tuberculosis.
http://www.pjms.in/index.php/panacea/search/search - Prof Dr Sumer Sanjiv Choudhary
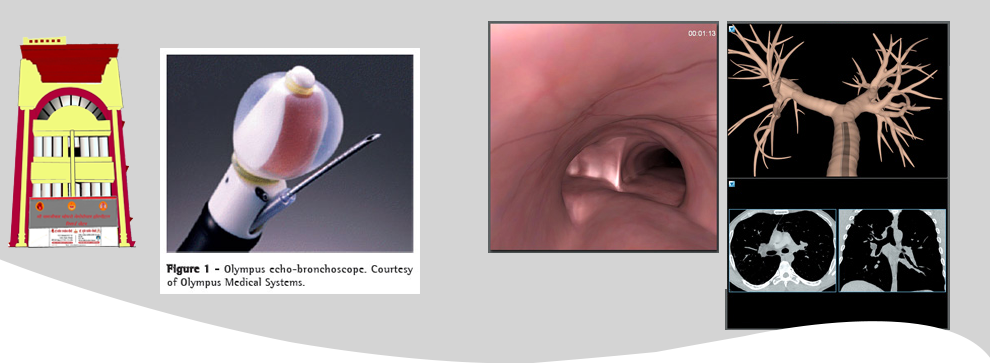
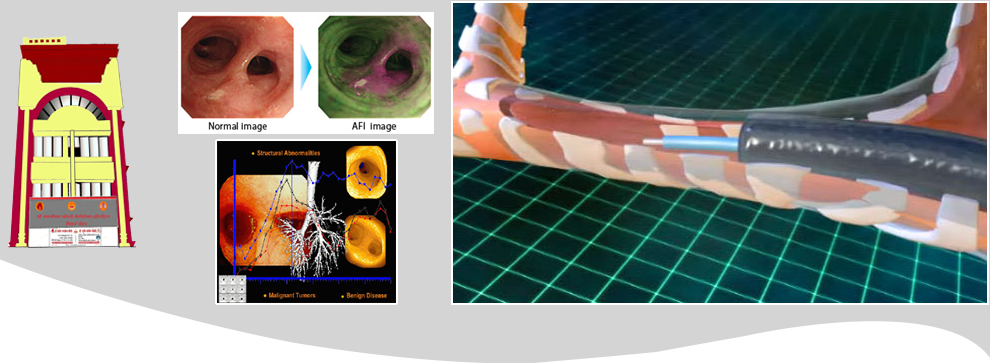
13. Outcome of fiber optic bronchoscopy in sputum smear negative pulmonary tuberculosis
Prof Dr Sumer Sanjiv Choudhary, BO Tayade, Shahank Kharbade, Anil Sontakke, Shaifee Khan, Rini Abraham
ABSTRACT
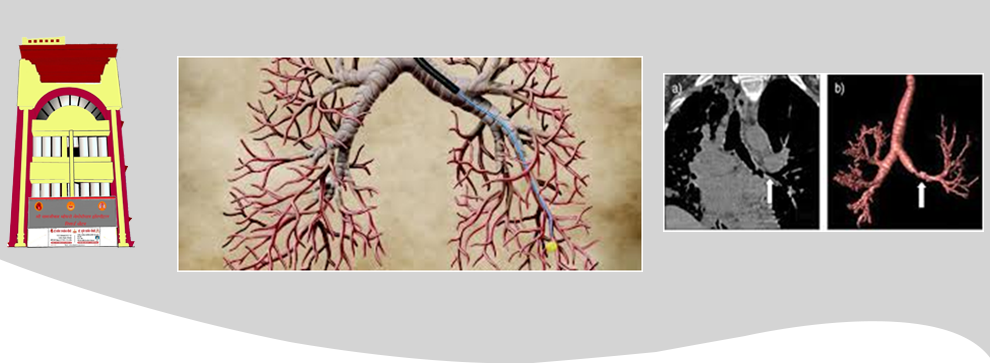
Bronchoscopy is very useful for diagnosing Sputum smear-negative pulmonary tuberculosis (SSN-PTB). Our aim is to find out the diagnostic yield of fiber optic bronchoscopy in sputum smear negative under RNTCP and radio logically suspected new cases of pulmonary tuberculosis and the complications of fiber optic bronchoscopy. A cross-sectional prospective study in which consecutive 108 patients was carried out in patients whose two sputum smear for Acid Fast Bacilli was negative and chest X-ray suggestive of pulmonary tuberculosis were included into the study. Fiber optic bronchoscopy was carried out in all patients. The yield for tuberculosis was 78 %( 85/108) i.e. made a final diagnosis of tuberculosis.29 (26.85%), 41(37.96%) and 30(27.78%) patients had positive AFB smear on Bronchial brush, Broncho alveolar lavage and post bronchoscopy sputum of which 11(12.94%), 22(25.88%) and 13(15.29%) patients had exclusive diagnosis from the respective procedures. The immediate yield combining positive smear samples from different procedures and histopathological evidence of caseating granuloma in present study is 56%(61/108). In Broncho alveolar lavage culture 57/108(57.08%) were confirmed tuberculosis diagnosis and 24(28.4%) patients had exclusive diagnosis on bronchial culture. Bilateral, advanced, and non cavitatory disease had 52, 53 and 64 patients diagnosed as pulmonary tuberculosis and was more as compared to different site, extent and type of disease on chest x-ray which were initially negative for tuberculosis. Our study suggests that fibre-optic bronchoscopy and its procedure can provide excellent material for early as well as confirming the diagnosis in suspected patients of pulmonary tuberculosis when smears of expectorated sputum do not reveal mycobacteria and helps in diagnosing different diseases and disorders having clinical picture mimicking tuberculosis.
14.CAT Score in Chronic Obstructive Pulmonary Disease, Impact on Health: Assessment in Our Region
Prof Dr Sumer Sanjiv Choudhary, Abraham Rini, Tayade B, Shafee Khan, Virag Doshi, Vishal More
ABSTRACT
COPD is a disease state that causes lot of human suffering, is now recognized as a common disease in developing countries and is one of the fastest growing chronic cause of death. Pulmonary function tests are essential for the diagnosis and evaluation of the severity of COPD but other measures of functional status such as dyspnoea, exercise performance and health status are important components of COPD that cannot be measured by this method. The COPD assessment test (CAT) is a new eight-item specific questionnaire and is intended to provide a short, simple and self-administered test for evaluating symptoms, in assessing the impact of COPD on health status (Quality Of Life) .This study shows the usefulness of CAT score in our region. The clinical characteristics, Gold Severity and FEVI 1 % of present study were compared with earlier studies of different countries. Total 70 patients with COPD were studied from May 2014 to September 2014. Detail clinical history was obtained. Assessment of symptom severity was made based on the CAT questionnaire. They were subjected to pulmonary function test (pre and post bronchodilator therapy) and oxygen saturation measurement. Majority of the patients were Male 42(60%). Total 41(58.6%) patients were smokers of which 36 (87.8%) were males. 18(25.7%) patients had positive history of Chula exposure of which 17(94.4%) were females Mean age of patients was 60.3 years SD 9.9, Mean FEV1 62.33 SD 18.2, and SPO2 94.2 SD 2.27. Patients were classified into two groups. Group 1 of low symptoms having CAT Score <10 and high symptoms Group2of patients having CAT score >10. More than half of the patients 80% had a high CAT score of >10 of Group 2. Most of the patients were of moderate obstruction50%. Patients in whom Forced expiratory volume in 1 s percent (FEV1%) predicted was significantly decreased had a significantly increased the CAT score (t = 2.67 p= .009). Patients with severe stage of the disease (as GOLD criteria) had high CAT score i.e. have a positive correlation whereas CAT score and FEVI % had inverse co relation. The mean FEV1% predicted was similar to France where as high compared to Germany, Netherlands, Spain and USA and lower than Belgium. The CAT questionnaire proves to be a sensitive test in detecting COPD health status as a simple and reliable tool. By the help of CAT questionnaire the patients and clinician’s awareness of COPD would be improved to make an early diagnosis thus providing a useful and objective tool for early recognition and long-term clinical and therapeutic monitoring of COPD patients especially in the clinical settings where spirometry is not yet available.
http://www.pjms.in/index.php/panacea/search/search - Prof Dr Sumer Sanjiv Choudhary
15.Chronic Obstructive Pulmonary Disease: The future
Prof Dr Sumer Sanjiv Choudhary
ABSTRACT
Chronic obstructive pulmonary disease (COPD) is one of the major causes of morbidity and mortality across the world. Almost 90% of COPD deaths are occurring in low and middle - income countries.(1,2)
Chronic Obstructive Pulmonary Disease (COPD) is a common, preventable and treatable disease that is characterized by persistent respiratory symptoms and airflow limitation that is due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.(3) This refined definition includes the impact of symptoms and developmental origins.
Chronic Obstructive Pulmonary Disease (COPD) is currently the fourth leading cause of death in the world but is projected to be the 3rd leading cause of death by 2020. The Global burden of COPD is estimated to be 384 million with a global prevalence of 11.7%. Females are at a higher risk of developing the disease with equivalent exposure as compared to males.
COPD is now not an untreatable disease, over the past few decades management have improved drastically with research growing exponentially. COPD was considered predominantly a smoking-related disease, however 25%–45% of patients suffering from the disorder have never smoked. The risk factors attributed to the disease that can affect at different life stages are —in utero due to maternal smoking/exposure to air pollution, in childhood because of respiratory tract infections and in adulthood due to indoor biomass fuels, outdoor air pollution.
In India, 90% of rural population houses and 32% of urban population houses cook their meals on a biomass stove,(4,5) only 25% of the cooking being done with cleaner alternative gases,(6,7) indicating biomass fuels a major cause of COPD. Mosquito coils used in the night are emitting particulate matter equivalent to around 100 cigarettes is also a major risk factor for development of non-smokers COPD.(8)
Lack of awareness of the disease, its symptoms or implications is one of the major reasons that the people at risk are not seeking help from their primary care physicians. Even if a symptomatic patient visits his general practitioners, there is increases chances of under diagnosis as spirometries are not routine and diagnosis is largely symptom based. The inhalational devices are generally prescribed at the ‘terminal stage’ of the disease and these devices have a virtual stigma in rural setting.
It is now well appreciated that COPD is much more than the combination of chronic bronchitis and emphysema. Chronic lung inflammation and remodeling of small airways can produce COPD, even in the absence of bronchitic symptoms or radiographic evidence of emphysema. The refined ABCD assessment tool adopts three step approach 1) diagnosis based on FEV1/FVC <0.7, 2) Airflow limitation assessment 3) Assessment of symptoms and risk of exacerbation.(3)
Due to the complexity of COPD, patients are best managed by a multidisciplinary team, which include clinicians, dietitians, educators, psychologist and respiratory therapists. The multidisciplinary team can educate patients to understand their disease and help in making self-management plans. TRILOGY is an important options in pharmacotherapy management for severe disease, bringing down the cost of treatment which still needs to be a priority in many parts of the world.(9)
Two Cochrane Reviews, one of admission avoidance hospital at home(10) and the other of early discharge hospital at home(11) were carried out on COPD patients. Higher admission rates were noted in patients of early discharge as compared to hospital at home. Fernando Martinez and colleagues report the results of the REACT trial, which shows that roflumilast, can reduce exacerbations and hospital admissions in patients with severe COPD and chronic bronchitis who are also receiving recommended therapy—a fixed inhaled corticosteroid and long acting β2agonist combination.(12)
We need to make protocols for the use of systemic corticosteroids, antibiotics, and, in hypercapnic individuals, noninvasive mechanical ventilation, which can accelerate recovery from exacerbations.
COPD patients frequently have co-morbidities like heart disease, osteoporosis, cachexia, and depression as result of or in conjunction with their COPD. These co morbidities severely impair the patient’s health status, quality of life and must be treated aggressively. In spite of optimal therapy, few of the patients will experience exacerbations requiring urgent care.
Clinical trials have proved that inhaled bronchodilators therapy along with pulmonary rehabilitation improve out come in terms of functional capacity and quality of life and may reduce mortality rates.(13,14) The benefit of oxygen supplementation has been proven in persons with severe resting hypoxemia, and lung volume reduction surgery is recommended for a subgroup of emphysematous patients.(13-15) The availability of effective treatments makes early intervention increasingly important. Pneumococcal and Influenza vaccination prevents lower respiratory tract infection and may reduce the infective exacerbations.
Despite of all our efforts, some patients will die due to COPD. Hence the, end-of-life issues should be discussed with patients and their families, especially in advanced disease, before they face a life-and-death crisis. This will ensure that the patient knows what would happen and patient’s wishes can be respected during periods of medical crisis.
Scientific research is advancing rapidly. After decades of modest progress, researchers currently are making rapid advances using modern methods of genetics, genomics, and molecular pathology to better understand COPD.(13,14) These new advances in knowledge show the importance of protecting young, developing lungs from insults, including tobacco smoke The renewed interest in COPD research provides hope that novel therapies with the potential for modifying the disease process will soon be identified.
All guidelines aim to improve health care processes and outcomes through minimization of practice variation, and optimization of resources.(16) In low and middle income countries, with resource limitations, future research initiatives should be considered on how to improve compliance, adherence, accessibility and implementation of new treatments, where the burden of COPD disease is great.
http://www.pjms.in/index.php/panacea/search/search - Prof Dr Sumer Sanjiv Choudhary
16.Study of patients with restrictive spirometry having significant bronchodilator response
Prof Dr Sumer Sanjiv Choudhary., Tayade B.O., Rini Abraham., Vishal More., Anchit Bhatnagar and Sonal Arsude
ABSTRACT
Introduction: Obstructive airway disease is characterized by reversibility on bronchodilator therapy measured by pulmonary function tests; however this is not often seen is restrictive diseases. We studied the clinical significance of bronchodilator reversibility in patients of restrictive pattern of spirometry. Materials and Methods: 30 patients with restrictive spirometry having significant bronchodilators response, were included in our study. Restiction was defined as decreased FVC and FEV1, with normal FEVI/FVC and a bronchodilator response as improvement of 12% and 200ml in FEV1 and FVC. Patients demographics, clinical history, treatment history, X-Ray characteristics, spirometry, diffusing lung capacity, and lung volumes measurements on Body Plethysmography were recorded. Results: The mean age was 48.60 + 14.06 years, majority of the patients were male 70 % and 22.23 + 3 .59 was females BMI slightly higher than males .40% were smokers, with shortness of breath the most common symptom, followed by cough, wheeze and chest pain..Asthma was the most common diagnosed medical condition and most of them were on bronchodialtors. The mean post bronchodilator FEV1% and FVC% was 66.88 + 24.28 and 70.95 + 24.99, with a reversibility of 12.91%.The FEV1/FVC% was 96.80+16.95. The mean TLC was normal whereas the RV, TLC, RV/TLC was increased. Conclusions: It can be concluded that post bronchodilator reversibility in patients of restrictive spirometry may be because of decrease elastic recoil resulting in early airway closure leading to air trapping and low FVC. Even though the numbers of such patients are low if symptomatic they would be benefited with bronchodilator therapy.
17.COPD, A RISING CONCERN FOR NON SMOKERS! IS IT TRUE?
Sumer Choudhary, Jaydeep Nayase., Shubham Telang and Tayade B.O.
ABSTRACT
Introduction: Chronic obstructive pulmonary disorder is the leading cause of morbidity and mortality worldwide. In clinical practice non smokers COPD patients are on rise, the risk factors which are important in its development were evaluated
Methods: This observational cross sectional study included a total 298 patients, with age above 18 years, diagnosed clinically and on spirometry as per Gold guidelines fulfill inclusion criteria.
Results: Of the 298 patients 150(50•34%) were nonsmokers and 49•66%) were smokers. Males were the predominant gender, most of them more than 60 years, with comparable mean age.COPD were found at an early age in smoker’s population. Most of the patients in non-smokers group had moderate obstruction (73•34%).Statically significant risk factors identified were occupational exposure (86•67%),education level (55•34%), biomass exposure (39•34%),associated conditions of pulmonary tuberculosis (22•67%) and chronic asthma (16%)(P<0•001). Other risk factors like outdoor air pollution (70%), childhood admissions (13•34%) though not statistically significant, contributed in development of non-smokers COPD. BMI in non-smoker’s population was lower than smokers 22.08+2.11. Most of the patients 50 (84•75%) of non-smokers population having biomass exposure had index more than sixty. Patients were classified according to gold stage and compared. The predominant gender was male in both groups with almost similar mean age and most of them above sixty years. The Gold Stage II+ group had higher outdoor air pollution (95%), occupational exposure (17•5%), biomass exposure (47•5%), passive smoking years 28 + 0•75 P < 0•001).
Conclusion: It can be concluded that significant proportion of COPD patient in our region and early diagnosis can be made by identifying the risk factors
http://journalijcar.org/issues/copd-rising-concern-non-smokers-it-true - Prof Dr Sumer Sanjiv Choudhary
18.Systemic lupus erythematous (sle) with hydro pneumothorax: a rare case report
Prof Dr Sumer Sanjiv Choudhary., Samruddhi.B.Tayade and Nalini .R. Humaney
ABSTRACT
Introduction: SLE an autoimmune disease, also known as lupus in which immune system affects healthy tissue of various regions of the body i.e. a multiorgan disease. Lung involvement is a common presentation in SLE; however life threatening pneumothorax is a rare occurrence in this disease. We describe a 26 year old young female diagnosed as SLE presenting with spontaneous pneumothorax. Intercostal tube was inserted and patient was given BIPAP ventilation and started on corticosteroids along with supportive treatment for underlying co-morbidities. Pneumothorax though not a common presentation in SLE can be life threatening with high mortality.
http://dx.doi.org/10.24327/23956429.ijcmpr20180499 - Prof Dr Sumer Sanjiv Choudhary
19.Unfamiliar happening of dermal tuberculosis over tattoo mark
Prof Dr Sumer Sanjiv Choudhary, Dr Preetam Dhande and Dr B
ABSTRACT
Introduction: Even though tuberculosis is a global epidemic with increasing prevalence, the number of dermal tuberculosis encountered in outpatient department is comparatively few. It can manifest itself due to endogenous or exogenous factors and present to us in variety of forms. Even if diagnosis is made confirmation is relatively difficult though advances in investigation techniques. Lupus vulgaris a type of skin tuberculosis a very rare phenomenon. Here we report a 23yr old engineer presenting with fungating growth atop tattoo mark, done few months back at a fair. Diagnosis was confirmed microbiologically as well as histopathology. Patient was started on anti-tubercular drugs following which his lesions subsided.
http://journalcmpr.com/issues/unfamiliar-happening-dermal-tuberculosis-over-tattoo-mark - dr Prof Dr Sumer Sanjiv Choudhary
20.Asthma control test (act) score: effectiveness, validation, reliability, and response in opd patients of our place
Prof Dr Sumer Sanjiv Choudhary, Jaydeep G Nayse, Dr B O Tayade, Dr Samrudhi Tayade,Dr Shriyansh Singh, Dr Preetam Dhande and Dr GopalGondchar
ABSTRACT
Introduction: The Asthma control Test (ACT), Asthma Control Questionnaires (ACQ) and GINA Scales are widely used clinical and scientific tool to evaluate asthma, but not yet validated nor reliability studied in different population Aims: Study is conducted to evaluate usefulness of ACT scores in initiation or treatment change in asthma patients, its reliability and to correlate ACT score with GINA guidelines and ACQ. Setting and Design: This hospital based cross sectional study at department of Pulmonary Medicine, NKP Salve Institute of Medical Sciences, Nagpur. Methods and Material: Our participants were patient’s age 12 years and above, asthma diagnosed according to GINA guidelines, literate to complete questionnaire. We compared ACT score with GINA asthma control, ACQ, and asthma severity. Statistical analysis used: EPI Info Software version 7. Results: Total 111 adult patients with new or previous diagnosed case of asthma who fulfilled the inclusion and exclusion criteria were included. The group of patients having ACT score >20 and < 15 had an agreement with GINA controlled and uncontrolled group. The group of patients having ACQ score of < 0.75 had fair agreement with ACT score >20.ACQ >1.5 had a moderate agreement with corresponding ACT score of < 20. The FEV1 % predicted had a positive correlation with ACT score Asthma control as defined by GINA was highly correlated with asthma severity. Most patients with severe persistent asthma were uncontrolled. Conclusions: Using appropriate cut off point’s agreement can be observed between numerical and categorical scale. The choice of the scale to evaluate current asthma control may have a significant impact on the control status of an individual patient.
http://journalcmpr.com/issues/asthma-control-test-act-score-effectiveness-validation-reliability-and-response-opd-patients - Prof Dr Sumer Sanjiv Choudhary
21.Discussion on: Determining the Impact of CAT Score in Chronic Obstructive Pulmonary Diseases
Patients Health in Our Region Chapter 1
ABSTRACT
Introduction: COPD is a disease state that causes lot of human suffering, is now recognized as a common disease in developing countries and is one of the fastest growing chronic cause of death. Pulmonary function Pulmonary function tests are essential for the diagnosis and evaluation of the severity of COPD but other measures of functional status such as dyspnoea, exercise performance and health status are important components of COPD that cannot be measured by this method. The COPD assessment test (CAT) is a new eight-item specific questionnaire and is intended to provide a short, simple and selfadministered test for evaluating symptoms, in assessing the impact of COPD on health status (Quality Of Life) .This study shows the usefulness of CAT score in our region. The clinical characteristics, Gold Severity and FEVI 1 % of present study were compared with earlier studies of different countries. Total 70 patients with COPD were studied between May 2014 to September 2014.Detail clinical history was obtained .Assessment of symptom severity was made based on the CAT questioanaire.They were subjected to Pulmonary function test (pre and post bronchodilator therapy) and oxygen saturation measurement. Majority of the patients were Male 42 (60%).Total 41(58.6%) patients were smokers of which 36 (87.80%) were males.18(25.7%) patients had positive history of Chula exposure of which 17(94.44%) were females Mean Age of patients was 60.34 SD 9.9, Mean FEV1 62.33 SD 18.2, and SPO2 94.26 SD 2.27. Patients were classified into two groups. Group 1 of low symptoms having CAT Score 10.More than half of the patients 80% had a high CAT score of >10 of Group 2.Most of the patients were of moderate obstruction 50%. Patients in whom Forced expiratory volume in 1 s percent (FEV1%) predicted was significantly decreased had a significantly increased the CAT score (t = 2.67 p= .009). Patients with severe stage of the disease (as GOLD criteria) had high CAT score i.e. have a positive corelation whereas CAT score and FEVI % had inverse co relation. The mean FEV1% predicted was similar to France where as high compared to Germany ,Netherlands ,Spain and U.S.A. and lower than Belgium. The CAT questionnaire proves to be a sensitive test in detecting COPD health status as a simple and reliable tool. By the help of CAT questionnaire the patients and clinician’s awareness of COPD would be improved to make an early diagnosis thus providing a useful and objective tool for early recognition and long term clinical and therapeutic monitoring of COPD patients especially in the clinical settings where spirometry is not yet available.
https://www.bookpi.org/bookstore/product/new-frontiers-in-medicine-and-medical-research-vol-8/ - Prof Dr Sumer Sanjiv Choudhary
22.HIGH FLOW NASAL OXYGEN- ALL YOU SHOULD KNOW
ABSTRACT
Introduction: Respiratory support is applied to maintain adequate oxygenation and ventilation and hence supplemental oxygenation is the first line of treatment for hypoxemic respiratory failure. There are multiple conventional oxygen support devices. However, in majority of these, oxygen provided is not humidified and maximum flow rate is 15l/min. However, high flow nasal oxygen (HFNO) is an alternative to conventional oxygen therapy. It is a technique that delivers heated and humidified oxygen with a controlled fraction of inspired oxygen(FiO2) at a maximum flow rate of 60L/min via (1) a specialized nasal cannula. Use of HFNO for acute respiratory failure has been considered for more than a decade now. Although it came into limelight for adults during the last two years when ICU beds and ventilators got occupied by the havoc of COVID-19 pandemic and it is during this time that HFNO came a lot handy. Thus, the purpose of this article is to provide the clinicians recent information about HFNO and to discuss it's pros as well as cons.
https://www.worldwidejournals.com/paripex/issues.php?m=October&y=2021&id=124 - Prof Dr Sumer Sanjiv Choudhary
23.Efficacy and Safety of Inosine Pranobex in COVID-19 Patients: A Multicenter Phase 3 Randomized
Double-Blind, Placebo-Controlled Trial
ABSTRACT
Introduction: Inosine pranobex (IP), an immunomodulatory agent, is used in the treatment of various viral infections. The results of a phase 3 randomized controlled trial are reported, evaluating the efficacy and safety of IP in the treatment of mild to moderate COVID-19. It includes 416 symptomatic patients with confirmed SARS-CoV-2 infection. In addition to a defined standard of care, patients randomly (1:1) receive either IP 500 mg tablet (IP group) or a matching placebo (placebo group) at 50 mg kg−1 body weight/day rounded to the nearest 500 mg dose (maximum 4 g day−1) administered in 3–4 divided doses for 10 days. Compared to the placebo group, IP group shows significantly higher rates of clinical response (CR) and clinical cure (CC) on Day-6 for both non-hospitalized patients and the total population. IP group shows significantly earlier CR and CC with fewer adverse events and no mortality. Based on these findings and the fact that IP increases natural killer cell-mediated cytotoxicity of virus-infected cells as an early immune response to viral infection and enhances NKG2D ligand expression, it is concluded that IP should be started early to maximize the benefit in mild to moderate COVID-19 patients. (Trial registration number: CTRI/2021/02/030892).
https://onlinelibrary.wiley.com/action/doSearch?AllField=inosine&SeriesKey=23663987 - Prof Dr Sumer Sanjiv Choudhary
24.Pulmonary Manifestations in Rheumatological Diseases
ABSTRACT
Introduction: Pulmonary involvement complicates the various aspects of care in patients suffering from autoimmune disorders. The epidemiological data generated over the last 10 to 15 years have improved the overall understanding of the risk factors and pathophysiological mechanisms involved in pulmonary involvement in rheumatological conditions. Recent advances in genetics have provided superior insight into the pathogenesis of autoimmune diseases and the underlying pulmonary involvement. This review article provides a concise overview of the four most common rheumatological conditions associated with pulmonary involvement: systemic lupus erythematosus (SLE), dermatomyositis/polymyositis, rheumatoid arthritis (RA), and systemic sclerosis (SSc). The clinical, epidemiological, and genetic aspects of these diseases are summarized in this article with particular emphasis on the characteristic patterns of pulmonary involvement in radiological imaging and various treatment options for each of these autoimmune diseases and their lung manifestations
https://www.cureus.com/articles/113988-pulmonary-manifestations-in-rheumatological-diseases?utm_medium=email&utm_source=transaction - Prof Dr Sumer Sanjiv Choudhary
25.Miliary Tuberculosis with Acute Respiratory Distress Syndrome: A Deadly Combination
ABSTRACT
Introduction: A unique and deadly presentation of miliary tuberculosis is acute respiratory distress syndrome. In this case report, we present the case of a 22-year-old male patient who presented with a history of weight loss, appetite loss for eight months, and rapidly worsening dyspnea for 15 days, for which he was admitted to the intensive care unit. Chest X-ray and computed tomography (CT) of the thorax revealed bilateral miliary opacities. Routine blood tests revealed hyponatremia and leukocytosis. The patient was started on non-invasive ventilatory support, intravenous corticosteroids, and anti-tubercular therapy on clinical and-radiological suspicion of miliary tuberculosis. The patient was admitted for one month and started to show rapid recovery after initiating anti-tubercular and corticosteroid therapy.
https://www.cureus.com/articles/133286-miliary-tuberculosis-with-acute-respiratory-distress-syndrome-a-deadly-combination#!/ - Prof Dr Sumer Sanjiv Choudhary
26. A case of tubercular empyema with pyopneumothorax
ABSTRACT
Introduction: Pyopneumothorax is a common complication associated with tuberculosis, especially in patients with lung parenchymal cavitatory lesions. In this publication, we highlight the case of a 43-year-old female patient who presented with chief complaints of dry cough, left-sided chest pain, and dyspnea on exertion. An X-ray of the chest posteroanterior (PA) view, revealed a left-sided moderate pleural effusion with pneumothorax. Immediate intercostal chest drain (ICD) insertion was done and a pleural fluid cytology sample was sent which was suggestive of tubercular empyema and the patient was promptly initiated on anti-tubercular treatment to which she responded well and showed clinical and radiological improvements.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10451592/ - Prof Dr Sumer Sanjiv Choudhary
27. Chronic Tubercular Mediastinitis: A Rare Case Presentation With Subcutaneous Emphysema
ABSTRACT
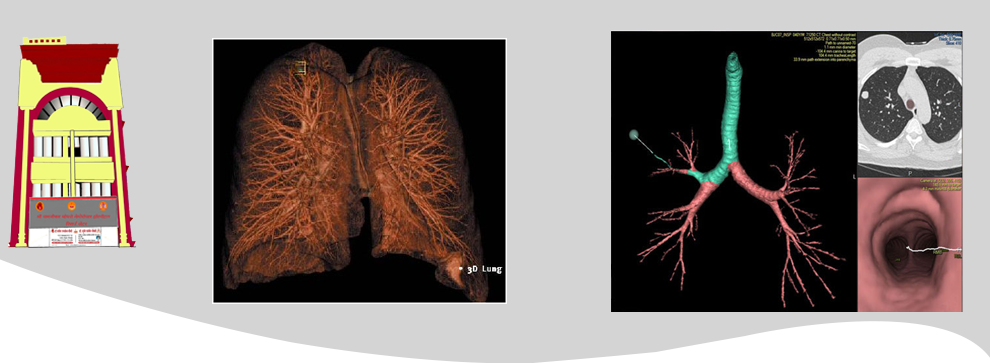
Introduction: Tuberculosis, histoplasmosis, various fungal infections, malignancy, and sarcoidosis are the most common causes of chronic or slowly progressing mediastinitis. Chronic mediastinitis of tubercular origin with subcutaneous emphysema is exceptionally uncommon, and the majority of cases are caused by trauma. Here we report the case of a 35-year-old chronic alcoholic male who presented to the Outpatient Department (OPD) with complaints of cough, chest pain, loss of weight, and intermittent low-grade fever for three months with no significant past medical history or family history for any respiratory diseases. He was admitted and all routine investigations were performed, which were normal including his chest X-ray, except erythrocyte sedimentation rate (ESR) which was raised. The patient's high-resolution Computed Tomography (HRCT) of the thorax was done which showed multiple pleural-based nodular lesions with few showing central cavitary nodules along with ground glass appearance. It also showed two fistulous tracks of 3.4-millimeter diameter, arising from the trachea at the T1 - T2 vertebral level and at the carina which led to the presence of air in the subcutaneous plane extending from the neck up to visualized abdomen suggestive of chronic mediastinitis with tracheal fistula, along with subcutaneous emphysema. This fistula was confirmed by video bronchoscopy as well as three-dimensional (3D) virtual bronchoscopy. A biopsy was taken, which was positive for acid-fast bacilli (AFB) stain, polymerase chain reaction (PCR) for tuberculosis, and positive tuberculin skin test. The patient was started on anti-tubercular treatment and on a follow-up visit upon completion of the intensive phase, his HRCT and video bronchoscopy showed fibrosing scarring with fistula closure.
https://www.cureus.com/articles/141717-chronic-tubercular-mediastinitis-a-rare-case-presentation-with-subcutaneous-emphysema#!/ - Prof Dr Sumer Sanjiv Choudhary
28. Post-tubercular Unilateral Lung Destruction: A Complicated Case
ABSTRACT
Introduction: Pulmonary tuberculosis is associated with long-term complications that affect both the respiratory and cardiovascular systems. We present the case of a 65-year-old male patient who presented with chief complaints of productive cough and breathlessness for the last four years. Further radiological investigations revealed a left-sided destroyed lung with left lung collapse and deviation of the mediastinum towards the left side. The patient responded well to treatment with broad-spectrum antimicrobial drugs and mucolytics.
https://www.cureus.com/articles/137025-post-tubercular-unilateral-lung-destruction-a-complicated-case#!/ - Prof Dr Sumer Sanjiv Choudhary
29.Sputum Culture Conversion among Patients with Drug‑Resistant Tuberculosis: A Study of Various Predictors.
ABSTRACT
Introduction: Introduction: Conversion of a positive sputum culture to a negative culture is an important parameter in the management of drug‑resistant tuberculosis (TB), as the failure to convert was related to dismal posttreatment outcomes and elevated mortality rates by almost eight times when compared to victims of multidrug‑resistant TB (MDR‑TB) who did so. In the patients of MDR‑TB, it is an important sign of treatment success to have sputum culture converted from positive to negative, and helps in determining the duration of treatment. The goal of this study was to examine and compare the length of time it took to convert an initial sputum culture with predictors of treatment outcomes for patients with MDR‑TB, as well as to pinpoint the variables that affected the length of time. Materials and Methods: The mixed method (records review and qualitative approach) was used to understand the patient’s perspective for accepting the Programmatic Management of Drug‑resistant TB (PMDT) services and the provider’s perspective for rendering services in a public‑private mix model setup. This study was undertaken as a retrospective analysis and studied the patients drug‑resistant TB who were admitted to a tertiary care hospital in central India. This study was carried out on the patients of Rifampicin‑Resistant TB (RR‑TB) and MDR‑TB (Resistant to both INH and Rifampicin) with positive baseline culture, pretreatment evaluation, and appropriate anti‑MDR‑TB treatment. As per the PMDT guidelines, sputum smear and culture reports were collected and analyzed. Results: In this study, the time and predictors to convert an initial positive sputum culture to negative and factors influencing treatment outcome were evaluated, compared, and identified. A total of 163 patients were evaluated and analyzed. Of these, 111 (68.09%) were rifampicin and INH‑resistant (MDR‑TB), whereas 52 (31.90%) were rifampicin resistant (RR‑TB) only. Overall 68 (41.71%) patients with baseline positive culture were converted within 3 months. Conclusions: It was concluded that malnourishment,human immunodeficiency virus positivity, associated extra pulmonary TB, and bilateral cavitation were found to be significant predictors of longer time of sputum culture conversion and thereby treatment outcome.
https://journals.lww.com/dmms/fulltext/2023/18020/sputum_culture_conversion_among_patients_with.14.aspx - Prof Dr Sumer Sanjiv Choudhary
30. Left-sided fibrothorax: a sequela of chronic tubercular empyema
Clinical image
https://pubmed.ncbi.nlm.nih.gov/38854864/ - Prof Dr Sumer Sanjiv Choudhary
31. The Role of Continuous Positive Airway Pressure (CPAP) Therapy in Obstructive Sleep Apnea With Metabolic Syndrome: Does It Affect the Outcomes?
ABSTRACT
Background: Of all fatalities occurring globally each year caused by noncommunicable diseases, obstructive sleep apnea (OSA) and obesity are associated with an increased risk of sudden death and cardiovascular mortality. Metabolic syndrome and its comorbidities are linked to OSA. The three essential elements of the metabolic syndrome are improper lipid metabolism, hypertension, and insulin resistance. The effect of continuous positive airway pressure (CPAP) on metabolic syndrome elements and related symptoms and whether CPAP therapy helps reverse the syndrome was studied.
Methods:The present study is prospective pre-post research conducted at a tertiary care center in Nagpur, Hingna, India. The cases included were of moderate to severe or worse OSA, older than 18 years, willing for CPAP therapy with no previous or current CPAP therapy. They had a history of excessive drowsiness during the day. The cases excluded from the study were those with an active, persistent breathing ailment requiring treatment, intervention, or diagnosis of dyslipidemia, diabetes mellitus, or hypertension, past or present, or evidence of damage to the vital end organs. Components of the metabolic syndrome were assessed at the beginning and end of three months of CPAP therapy.
Findings:Eighty-five cases were enrolled in the study, of which 79 completed it. The majority of cases were male, comprising 48 individuals, accounting for 60.8% of the total cohort. Additionally, 54 cases, representing 68.4% of the group, had hypertension. The average age of the participants was 53.95 years ± 6.84 years. The BMI mean was 30.4 kg/m2 ± 4.642, with a waist-hip ratio of 0.964 ± 0.056 and a neck circumference of 40.66 cm ± 3.37. The study population scored 12.53 ± 2,616 on the Epworth Sleepiness Scale. The study population’s apnea-hypopnea index/respiratory disturbance index ratio was 16.118 ± 4.868, a moderate risk score. After three months of CPAP therapy, there was a significant improvement in glycated hemoglobin (HbA1c), tetraiodothyronine (T4), high-density lipoprotein (HDL), and oxygen desaturation, and they were also statistically significant. In the study group, there was a decrease in systolic and diastolic blood pressure of 2.21 mm Hg and 0.26 mm Hg, respectively. Other indicators, including HbA1c, fasting and post-meal blood sugar, triglycerides, and HDL cholesterol, were significantly lower. We observed in the less than 50-year-old age group better improvement in systolic blood pressure of 0.49 mm Hg, diastolic blood pressure improvement of 0.32 mm Hg, and fasting blood sugar improvement of 14.59 mg/dl, and in the age group of more than 50, better improvements in post-meal blood sugar of 9.7 mg/dl, along with a statistically significant change in triglyceride with an improvement of 16.26 mg/dl, P value less than 0.05.
Interpretation:After three months of CPAP therapy, there was a significant improvement in HbA1c, T4, HDL, and oxygen desaturation, and they were also statistically significant. Fourteen (17.72%) cases of post-CPAP therapy no longer met the requirements for the syndrome. There was an improvement in the blood pressure’s diastolic and systolic values, fasting and post-prandial sugar levels, HbA1C, and triglyceride levels. Patients over 50 years old showed better improvement in post-meal and triglyceride levels. Females improved blood pressure and triglycerides, whereas males responded better to blood sugar levels.
https://www.cureus.com/articles/228266-the-role-of-continuous-positive-airway-pressure-cpap-therapy-in-obstructive-sleep-apnea-with-metabolic-syndrome-does-it-affect-the-outcomes#!/ - Prof Dr Sumer Sanjiv Choudhary
32. Lipoid Pneumonia Secondary to Diesel Aspiration: An Occupational Hazard.
ABSTRACT
Introduction: Lipoid pneumonia is defined as a type of pneumonia that occurs as a result of inhalation of either endogenous or exogenous lipid-containing products in the lungs. We present the case of a 55-year-old male patient who presented with chief complaints of cough with blood-tinged sputum, right-sided chest pain, dyspnea, and fever for two days. The patient gave a history of working as a mechanic in an automobile garage and reported an episode of accidental aspiration of diesel during diesel siphoning at the workplace. A chest X-ray and computed tomography (CT) scan of the chest were done, which revealed right-sided lower lobe consolidation. The patient was admitted and started on intravenous antibiotics, corticosteroids, and inhaled bronchodilators, along with oxygen support. A bronchoscopy was done, which revealed the presence of thick mucoid secretions in the right lower lobe bronchus. The patient was discharged after 10 days with stable vitals and was advised to have regular follow-ups to monitor for any long-term pulmonary complications.
https://www.cureus.com/articles/239049-lipoid-pneumonia-secondary-to-diesel-aspiration-an-occupational-hazard#!/ - Prof Dr Sumer Sanjiv Choudhary